| |
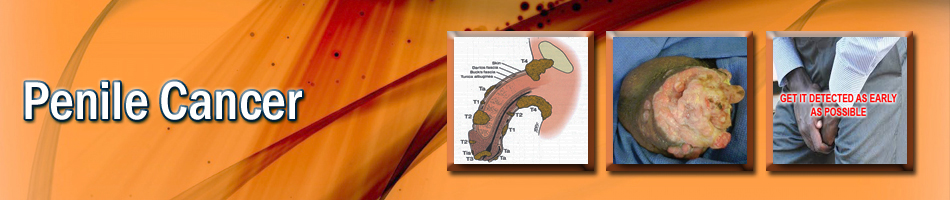
| Penile Cancer |
|
|
Malignant tumors of the penis are thankfully rare in the United States. But would you know how to recognize this cancer? The following information should help you spot this tumor long before it becom |
| |
|
What causes penile cancer? |
|
|
Scientists currently believe that penile tumors are caused by cancer-producing effects of secretions that become trapped within the foreskin if they are not washed away on a regular basis. It is not surprising, therefore, that this particular malignancy is extraordinarily common in South and Central America, and Third World countries, where public health and personal hygiene often are lacking. Also, circumcision, a practice that could improve hygiene, is not regularly performed. In the United States, penile cancer is a relatively unusual cancer, probably due to the country's superior sanitary and hygienic conditions along with commonly practiced circumcision.
However, scientists are currently studying other causes of penile cancer, particularly the role of human papilloma virus (HPV), which already has strong links to cervical cancer. Antibodies to HPV-16, a specific type of papilloma virus also implicated in cervical cancer, have been found in many patients with penile cancer. |
| |
|
How is penile cancer diagnosed? |
|
|
Unfortunately, early diagnosis of penile cancer is often missed because it is so rare in the United States that general physicians and even urologists may only see two or three cancers in a practice lifetime. Also, patients are often reluctant or embarrassed to call attention to their genitalia and may be afraid of surgical procedures or treatment of the penis.
But the earlier the diagnosis, the more effective the therapy and the better the chance for cure. If diagnosis is delayed and the disease progresses, therapy may be less successful and more disfiguring. So, it is very critical that any skin erosion, ulcer, sore, irritation, discoloration that is noticed on the foreskin, the skin of the shaft of the penis or the surface of the head of the penis be brought to the attention of the physician by the patient and be promptly evaluated.
Chances are good that most such lesions are linked to a bacterial or fungal infection or even an allergic reaction, all of which will respond readily to antibacterial or antifungal ointments and creams. But growths or areas that return or do not heal must be considered malignant until proven otherwise. The appropriate evaluation includes biopsy where the tissue is removed for examination under a microscope.
If a precancerous or cancerous condition is found, prompt treatment and systematic, regular follow up are very important. |
| |
|
How is penile cancer treated? |
|
|
Early detection and identification of penile cancer are very valuable because the treatments that can provide successful outcome are indeed low risk. If the tumor appears on the skin surface, your urologist may be able to treat the problem with a topical cream that has minimal side effects.
If the lesion is larger, but still limited to about pea-size, a small local excision or a type of surgery that continues to shave layers of abnormal tissue until normal tissue is reached (Moh's surgery) may be performed. With these procedures, there is essentially no loss of form or function to the penis. However, careful follow up is critical to identify early recurrence. In the removal of these small lesions, it is very unlikely that cancer has spread to lymph nodes and, therefore, removal of the lymph nodes is usually not necessary.
With larger lesions, it is necessary to remove greater amounts of tissue and also to consider removal of the draining lymph nodes in the groin in order to achieve a cure. In these circumstances, a combination of surgery, radiation and chemotherapy may be necessary.
It is also important to note that external beam radiation is an alternative therapy, specifically for small lesions. Again, the critical importance of early detection not only ensures a better outcome for the treatment supplied but also provides more treatment options that can be applied. |
| |
|
What can be expected after treatment for penile cancer? |
|
|
Your post-treatment experience will be directly tied to the stage of your cancer when it is diagnosed. Cure is almost certainly ensured when lesions are detected early. But it is less certain as the tumor becomes more advanced. Treatment is also increasingly more debilitating. Since your penis is readily accessible — you can visualize it easily and you touch it regularly during urination — you can help yourself greatly in detecting early disease by reporting any lesions that you see or feel. While patients at greatest risk are those who are not circumcised, every man should be on the lookout for penile lesions as they need prompt attention.
|
| |
|
| Frequently asked questions: |
| |
Is penile cancer contagious? Can I pass it onto others? |
|
|
Until recently, the general consensus was that penile cancer was caused by chemical irritation and there was no concern about transmitting it. But recent data have implicated the HPV in both penile and cervical cancers. There appears to be increased incidence of these cancers in the spouses of people with this sexually transmitted disease. Thus, while penile cancer is not directly transmissible, if you or your partner has HPV, you need to use protection during intercourse, be aware of any lesions, and, if you are the woman, have frequent cervical examinations. Not only are efforts to eliminate or minimize the infection important but so are discussions with a urologist or other specialist about its link to penile cancer. |
| |
|
Does an operation on the penis mean that I will be unable to stand to empty my bladder? |
|
|
If your cancer is detected early, the surgical procedures should not impact your ability to stand when you urinate. When the cancer is more advanced, the required surgical procedures may require you to urinate in the sitting position.
Will treatments interfere with my ability to have sex?
Early detection and minimal surgical procedures should not interfere with normal sexual function. More extensive procedures might, however. |
| |
|
Should all male children be circumcised soon after birth to prevent penile tumors? |
|
|
This question creates much debate. Some experts believe that sexual sensation is diminished after circumcision, even though evidence points to a lower incidence of urinary tract infections and penile cancer in men who have had the procedure. Parents should discuss the risks and benefits of circumcision with the child's doctor.
|
| |
|
If a male has not been circumcised soon after birth, will later circumcision as a teenager or young adult protect him from penile cancer? |
|
|
There is now evidence that circumcision soon after birth is the most reliable protection from subsequent penile malignancies. A procedure performed in young adults does not have nearly the protective effect as when it is done in infants. Population studies suggest, for instance, that the incidence of penile cancer is:
» extraordinarily rare in Jewish males where circumcision at birth is an accepted ritual.
» more common in the Muslim population where circumcision at puberty is the established ritual. But it is not as common as in those individuals who have never been circumcised |
| |
|
| |
|
| |
|
|
 |
Endoscopic removal of urinary stones: PCNL, URS, RIRS, CLT |
|
 |
LITHOTRIPSY (ESWL) |
|
 |
LASERS for stones and Prostate |
|
 |
Monopolar and bipolar TURP |
|
 |
HOLEP |
|
 |
Urodynamics and uroflowmetry |
|
 |
Laparoscopic urology surgeries |
|
 |
Paediatric urology surgeries |
|
 |
Urinary incontinence surgeries |
|
 |
Surgeries for genitourinary cancers |
|
 |
Reconstructive urology |
|
 |
Microsurgeries for infertility and impotence |
|
| |
|
| |
 |
| |
|
| |
| |
| |
| |
| |
| |
| |
| |
| |
|